top
 Fertility Therapies Fertility Therapies
ขั้นตอนการใช้เทคนิค
ช่วยในการตั้งครรภ์ใน
สตรีที่มีบุตรยาก
 Ovulation
Induction Ovulation
Induction
การกระตุ้นให้เกิดไข่ตก
 Artificial Artificial
insemination
การใช้สเปิร์มฉีดเข้าใน
มดลูกหรือท่อรังไข่
 Assisted
Assisted
Reproductive
Technology. ART
เทคนิควิธีการผสมเทียม
- IVF
- GIFT
- ZIFT
- ICSI
 วิธีการทำการทดสอบ วิธีการทำการทดสอบ
การตั้งครรภ์
HCG Preganacy test
 วิธีการทดสอบหาวันไข่ตก วิธีการทดสอบหาวันไข่ตก
สำหรับผู้มีบุตรยาก
LH Ovulation
test
 Sample
Basal Body Sample
Basal Body
Temperature Chart
(BBT)
ตัวอย่างตารางวัดอุณหภูมิเพื่อ
หาวันไข่ตก





สนใจรายละเอียดเพิ่มเติม
กรุณาแจ้งให้ทึมงานเพื่อ
จัดเตรียมหาสาระให้
Contact :
info@thailabonline.com
ชมรมเรารักสุขภาพ
ไทยแล็ปออนไลน์


|
|
Your Guide: Anna Peris, PharmD. -Stadtlanders' Clinical
Fertility Specialist
เป็นขั้นตอนการใช้เทคนิคพิเศษทางการแพทย์มาช่วยในการตั้งครรภ์
โดยจะ
เป็นขบวนการหลังจากได้พยายามทำขบวนการขั้นต้นมาแล้วไม่ได้ผล
เช่น
การวัดอุณหภูมิหลังตื่นนอนในตอนเช้า การตรวจหาฮอร์โมน LH
เพื่อหาวัน
ไข่ตกก็แล้ว แพทย์ก็จะเริ่มพิจารณาในขบวนการนี้ต่อไป
เพื่อช่วยให้มีการ
ตั้งครรภ์ เรารวมเรียกขบวนการนี่ว่า
Assisted Reproductive Technology (ART: GIFT, ZIFT,
ICSI, and IVF)
If you've reached this point, you
and your partner have probably tried all the
"basic" methods to
enhance your chances of becoming pregnant. You've been monitoring
your cervical mucus secretions, measuring your basal
body
temperature (BBT), and perhaps even testing your urine
to predict ovulation.
Despite persistent attempts with
these simple strategies, you have yet to
achieve a
pregnancy. At this point, your doctor may have suggested one
of
several fertility therapies to maximize your chances of
getting pregnant. If you
feel confused and overwhelmed with
the options available to you, don't worry,
we are here to
help! -Anna
Introduction to Fertility
Treatments
Fertility treatments don't have to be as
complex as they may initially sound.
Millions of couples go
through these treatments every year. And although it is frustrating,
the most important thing you can do for yourself is to gain as much
knowledge as possible regarding each treatment option. You need to
feel comfortable with every step of the process and know what to
expect from a
medical, emotional, and financial
standpoint.
The purpose of this primer is to give you basic
information that you need about
fertility treatments in
general. Continue to follow the links for each
individual
treatment option to learn more in depth material
such as indications, side effects,
and success rates.
Remember, the more you know, the better you'll feel.
In
general, fertility treatments fall into one of three
categories:
ขั้นตอนการใช่เทคนิคเข้ามาช่วยในการตั้งครรภ์
จะมี 3 ขั้นตอนขึ้นอยู่กับว่า
การใช่ขั้นตอนแรกแล้วยังไม่ได้ผล
ก็จะขยับไปในขั้นต่อไป
จนถึงขั้นใช้วิธี
การผสมเทียมเป็นขั้นตอนสุดท้าย
ดังนี้
 Ovulation
Induction (OI) Ovulation
Induction (OI)
กระตุ้นให้เกิดการตกไข่
 Artificial Insemination (AI and IUI) Artificial Insemination (AI and IUI)
การใช้สเปิร์มฉีดเข้าในมดลูกหรือท่อรังไข่
 Assisted Reproductive
Technology (ART: GIFT, ZIFT, ICSI, and IVF) Assisted Reproductive
Technology (ART: GIFT, ZIFT, ICSI, and IVF)
ขบวนการใช้เทคนิคผสมเทียมช่วยให้เกิดการตั้งครรภ์
The
purpose of ovulation induction is exactly what the name says -
inducing the woman to ovulate. This is done with either a pill or
injectable medications.
Ovulation induction is
appropriate for certain women, depending on their
diagnosis
- it's not right for everyone. It usually works the best for couples
where
the woman can't get pregnant because she doesn't
ovulate regularly or
consistently. In some cases, a little
pill may be all that is needed to do the trick
(for more
information on fertility medication, see At The
Pharmacy).
The answer is not always so simple however.
Some couples may be more
suitable candidates for artificial insemination or
AI. AI means taking a purified specimen of the male partner's
sperm and injecting it into the female partner's reproductive tract.
In many cases, this may facilitate fertilization if a couple
is
unable to get pregnant. AI is certainly more involved
than ovulation induction - it requires an outpatient procedure and
monitoring the woman's response to
potent fertility
medications.
The most complex fertility procedures are
grouped under the name ART, which stands for Assisted Reproductive
Technology. There are several different kinds
of ART
procedures, including IVF, GIFT, ZIFT, and
ICSI. The basic concept
behind
ART is that involves taking the egg out of the female body in order
to
assist the process of fertilization. The simplest ART
procedure, IVF has been
around for over 20 years. Although
it is still being perfected, modern medicine
has come a
long way. In many cases, the ART procedures have helped hopeful
couples have many children.
ART, or any of the other
fertility treatments should be approached with careful
consideration. Although these therapies provide exciting
possibilities, it is
important to understand what each one
entails. Fertility treatments utilize potent medications and require
a significant emotional and financial commitment from
each
partner. Learn the most you can about your options, and ask
many
questions. It is critical to have all the information
you need up front, before you
initiate
therapy.
Discussions question
"I
have one child and shortly after his birth i became pregnent again.
I had a miscarriage during my third month. since ..."
-Talk About
It
Ovulation induction is a very common term that you
may encounter in your
journey through fertility treatments.
Basically, this term refers to the use of
medications to
stimulate your body to produce one or more eggs.
Ovulation
induction may be necessary in women who do not
ovulate consistently, but want
to have a child. There are
many reasons why women do not ovulate regularly - polycystic ovarian
syndrome (PCOS), excessive exercise, and
hyperprolactinemia
are just a few examples. One important prerequisite for
a
woman to participate in ovulation induction is that she
must have good quality
eggs remaining in her ovaries. This
procedure is of no use to women who have ovarian failure or eggs of
poor quality.
Ovulation induction can be as simple as
taking a daily pill or more complicated,
like injecting
fertility medications and seeing your specialist daily for necessary
monitoring. The simplest form of ovulation induction involves taking
clomiphene. Clomiphene is a small tablet that must be taken on
specified days of the cycle.
It is relatively inexpensive
and has very few side effects. If taken correctly, clomiphene can be
very effective in inducing ovulation. As many as 50-80% of women who
take clomiphene will ovulate, however only about half of these will
achieve a pregnancy.
In some cases, a woman may need a
little extra help in getting her body to
produce eggs.
Remember, not everyone is the same and therefore not
every
woman will necessarily respond to clomiphene. More
potent medications, known
as the gonadotropins, are
available for more intensive ovulation induction. Gonadotropins are
injectable medications that are made up of a combination of follicle
stimulating hormone (FSH) and luteinizing hormone (LH) or just FSH
alone. These hormones can be very helpful in getting a woman to
produce and release
her eggs. Because these medications are so
potent, you will be required to visit
your specialist's
office frequently to get appropriate monitoring and
guidance.
This can include bloodwork, ultrasounds, or just
verbal counseling in regards to dosing and injection techniques.
Close contact with your healthcare team will
ensure that
you get the best outcome from the treatment and also help prevent
potential side effects from the therapy.
For some
women, ovulation induction with medications will not be enough
to
achieve pregnancy. Even if the medications work, there
may be other reasons
that prevent the couple from becoming
pregnant - for example, a low sperm
count. For couples
where ovulation induction is unsuccessful in producing a pregnancy,
one of many ART procedures may be advised as the next path to
parenthood.
For the ART procedures, injectable
gonadotropin medications are also used to stimulate the woman's
ovaries to produce multiple eggs. However, when medications are used
in preparation for an ART procedure, the process is
no
longer called ovulation induction, but rather controlled
ovarian hyperstimulation
or COH. The only difference
between the 2 procedures is that in COH, the woman
is never
actually "allowed" to ovulate - rather, her eggs are retrieved from
the
ovaries immediately prior to the anticipated time of
ovulation (in the case of IVF)
and fertilized outside of
the body, in a laboratory. In ovulation induction, however,
ovulation is desirable since a natural pregnancy is being attempted.
COH
requires extensive monitoring and follow-up since it
involves the use of
injectable
gonadotropins.
The success of ovulation induction in
achieving a pregnancy is highly variable.
It depends on
your diagnosis, age, the medication being used, and
numerous
other factors. Therefore, it is important that you
speak with your specialist
regarding your anticipated rate
of success with a chosen treatment.
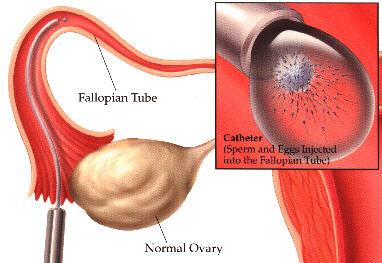
AI and
IUI
Discussions
Suffering from blocked fallopian
tubes
"Hi,
I am 27 and my husband and I have been trying to
have a baby for 2 years now.
No luck! In that time I have
had ma..."
-Talk About It
As a couple dealing with
infertility, you may be faced with various options in your journey
to become loving parents. Artificial insemination or AI is just one
of those options that may be considered prior to attempting more
involved treatments,
such as IVF. AI is typically
recommended for the treatment of infertility due to:
mild
to moderate male factor infertility
"unexplained"
infertility
cervical mucus insufficiency
hostile
cervical mucus
various structural abnormalities in the
woman
Many couples are presented with the AI option after a
trial of clomiphene is unsuccessful.
AI is a relatively
simple procedure that involves injecting a sample of specially
treated sperm from the male partner into the female partner's
reproductive tract.
For most couples, AI is performed with
the husband's sperm. However, when the husband's ejaculate contains
few or no live sperm, the couple may consider undergoing more
advanced procedures including IVF, ICSI, or donor sperm
insemination.
It's important to note that AI is a
general term - there are actually several different types of AI, and
they are named for the location of sperm insemination into the
female. The types of AI are intracervical (in the cervical canal),
intrauterine (in the uterine cavity), intrafollicular (in the
ovarian follicle) or intratubal (in the fallopian
tubes).
Therefore, AI merely describes a procedure where a
qualified
reproductive specialist injects sperm into the
female reproductive tract. The
different types of AI are
recommended based on your diagnosis and probability
of
success with each method.
Of the four different types
of AI, intrauterine insemination (IUI) is the most
commonly
used form. It is very useful if the cause of infertility is
insufficient or
hostile cervical mucus or low sperm count
or motility. The reason for this is IUI
allows sperm to
bypass the cervix without encountering "unfriendly"
cervical
mucus which could "inactivate" the sperm. The
reason that IUI is helpful for low
sperm count or motility
is based upon the knowledge that only about 1% of the
total
numbers of sperm deposited into the vagina at ejaculation will find
their way
into the upper female genital tract. IUI places
the healthiest sperm into the female genital tract to increase the
likelihood that one of those sperm will fertilize an
egg.
IUI is a relatively quick procedure that takes
place in the clinic office. It is
performed by passing a
sterile catheter containing the sperm through the
cervix
and into the uterine cavity. The sperm are then
injected directly into the uterus. Usually the insemination itself
causes little if any discomfort. Following the insemination
procedure, you will likely be asked to remain lying down with
your
hips elevated for about 45
minutes.
Although IUI is relatively uncomplicated, and
less invasive than IVF, one disadvantage associated with IUI is that
it does not allow the doctor to evaluate whether or not
fertilization is capable of taking place. With IVF/ET,
fertilization
can be confirmed since it takes place outside
of the body, in a lab. With IUI,
however, fertilization
still takes place within the body, much like a natural cycle.
Although IUI is more natural, it is unknown whether or not the sperm
actually
fertilizes the egg to make an embryo (unless the
woman gets pregnant after
the first IUI cycle). Therefore,
if you repeatedly are unsuccessful in achieving pregnancy following
IUI, consider discussing the IVF option with your healthcare
team.
The pregnancy rates for IUI treatment cycles
average about 15-20% per cycle
when IUI is performed for
the correct indications. If all other conditions
affecting
fertility are thought to be normal or adequately
treated, then a reasonable length
of treatment with IUI is
about three to six treatment cycles. If you and your
partner
are unable to achieve pregnancy by the end of this
course of treatment, then
speak with your doctors about
other options available to you. Perhaps a reassessment of your
diagnosis should be made since some other factor may
be
present which has been unrecognized and inadequately
treated.
ART stands for Assisted
Reproductive Technology. ART procedures include
IVF, GIFT,
ZIFT, and ICSI. ART procedures generally involve taking the egg
out
of the female body in order to assist the process of
fertilization. The simplest
ART procedure, In Vitro
fertilization -IVF
has been around for over 20
years and is perhaps the most commonly
recognized ART of
all procedures. I have developed a seperate section on IVF and will
focus our discussion here on GIFT, ZIFT, and ICSI.
-Anna
ZIFT
Depending on
your diagnosis, your doctor may discuss the option of performing
zygote intrafallopian transfer (ZIFT) instead of conventional IVF.
ZIFT may be recommended if the husband has severe male factor
infertility or if there has
been difficulty confirming
fertilization with past procedures. ZIFT has the advantages
of allowing fertilization to be confirmed and it has
demonstrated
higher success rates than IVF when used for
the appropriate indications.
ZIFT nothing more than a
variation of traditional IVF. With ZIFT, the fertilized egg that is
transferred back into the woman is allowed to divide only to the
2-cell
stage, instead of the 4 or 8 cell stage as with
conventional IVF.This fertilized egg at the 2-cell stage is
called a "zygote".
Like IVF, ZIFT involves ovarian
stimulation, monitoring, and egg retrieval,
followed by
sperm processing and fertilization in the laboratory. Another slight
difference between IVF and ZIFT (besides the stage of the
transferred embryo)
is the location where the embryos are
placed in the woman's body. With IVF, the embryos are placed
directly in the uterus. With ZIFT, however, the zygotes are placed
directly into the fallopian tube. Therefore, a criterion for
performing ZIFT
is that the female partner has at least one
open and functioning fallopian tube.
One disadvantage
with ZIFT is that the transfer of the zygote must be performed
through a laparoscope. This involves a surgical incision, whereas
with IVF, the fertilized eggs are transferred through the vagina
without the need for any
incisions. Although laparoscopy is
a minor surgical procedure, it still adds to the complexity, risk,
and cost of the entire process.
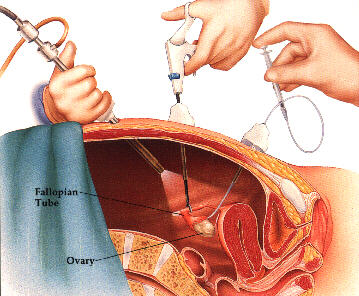
GIFT
Gamete intrafallopian transfer (GIFT) was
developing in 1984 as a variation of in vitro fertilization (IVF).
Your doctor may recommend GIFT if your diagnosis is unexplained
infertility infertility due to
immunological factors
endometriosis selected cases of male infertility tubal
infertility
A requirement for the procedure is that the
female partner having at least one
open (patent) fallopian
tube. GIFT is sometimes selected based on a couple's religious
beliefs that prohibit conception outside the body.
GIFT is
not much different than IVF. The main difference is that with GIFT,
fertilization occurs
naturally within the female partner's body instead of in the
laboratory as with IVF. GIFT involves ovarian stimulation,
and egg retrieval like IVF, but with GIFT, sperm and eggs are placed
directly into the woman's fallopian tubes to foster fertilization.
The following steps outline what you can expect when undergoing
GIFT:
Step 1: Ovarian
Stimulation and Monitoring
This step is exactly
the same as in IVF. In order to maximize the chances of success, the
physician will prescribe fertility medications (such us Humegon? or
Fertinex?) to stimulate the woman to produce more than one follicle
and egg.
HCG (Profasi? or Novarel?) is then typically given
to stimulate the release of the eggs from the follicles and time the
egg retrieval step.
Step 2: Egg
Retrieval and Sperm Processing
This step also
mirrors the process in IVF. The eggs are removed from
the
woman and examined under a microscope to evaluate
maturity before they are combined with sperm. The male semen sample
has been collected, evaluated, and sperm processing performed prior
to the next step.
Step 3: Gamete
Transfer
Once the physician has determined the
eggs are ready for transfer, the selected sperm and eggs are placed
together in a catheter. These sperm and eggs are called gametes. In
IVF, these gametes would be united in the laboratory by an
experienced embryologist, however this does NOT happen with GIFT.
With GIFT, the gametes are
injected into the fallopian tube using a special catheter
(laparoscope). Within the fallopian tube, fertilization will
hopefully occur naturally. Unlike IVF in which actual
fertilization is observed and confirmed in the laboratory, GIFT does
not allow visual confirmation of fertilization. If fertilization
occurs, the developing embryos remain in the fallopian tube and then
move to the uterus for the natural implantation
process.
For selected cases of infertility, GIFT may
have a higher success rate than IVF. This may be due to the fact
that GIFT more closely mimics natural conception as compared to IVF.
Specifically, the egg is fertilized in the fallopian tube rather
than
in the laboratory. In some cases, however, GIFT may
not offer additional advantages to IVF, but may in fact add to the
cost of therapy. Therefore, discuss with your specialist if you are
a good candidate for this procedure.

Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic sperm
injection, or ICSI, was developed to treat couples who previously
had a very poor probability of achieving fertilization due to the
male partner's extremely low numbers of viable sperm.This treatment,
when combined with in vitro fertilization, allows these couples a
more favorable probability of achieving conception. ICSI has
replaced the two previously developed micromanipulation techniques
of partial zona dissection, or PZD, and subzonal insertion, or SUZI,
because of the overall higher fertilization rates achieved with
ICSI. ICSI has revolutionized treatment for severe male factor
infertility because
the procedure requires only one healthy
sperm to potentially achieve fertilization.
A variety
of sperm problems can account for male infertility. Sperm can be
completely absent in the ejaculate, a condition known as
azoospermia. Men with low concentrations of sperm in the ejaculate
have a condition known as oligospermia. Poor motility, or a
condition called asthenospermia, occurs when
the sperm do
not have the forward swimming motion sufficient to make
the
journey from the ejaculation site in the female's
vagina, though the reproductive tract, to unite with the egg in the
fallopian tube. Men whose sperm have an increased percentage of
abnormal shapes and forms have a diagnosis of teratospermia. Other
sperm problems that prevent fertilization are
abnormalities
in the series of steps required for
fertilization, such as the sperm's ability to bind and penetrate the
cytoplasm of the egg.
Male factor infertility may be
caused by blockages, varicoceles, or abnormalities of the
ejaculatory ducts causing low or no sperm in the ejaculate. Men who
have had a severe injury to their male reproductive organs, some
neurological disorders, or surgery (including vasectomy), may have
an absence of sperm in
the ejaculate. Men who have had
radiation and chemotherapy treatments for cancer, may have low or no
sperm present in the ejaculate. Men who have provided semen samples
prior to undergoing cancer treatments and major surgeries of their
reproductive organs are candidates for ICSI due to the limited
number of sperm available to achieve conception with ART
procedures.
ICSI may be a recommended treatment option
for all of these infertile men.
Steps One: Ovulation Stimulation and
Monitoring
The same process used in the other ART
procedures to induce ovulation is
used with
ICSI.
Step Two: Sperm
Extraction
Semen samples can be obtained through
masturbation. If any viable sperm can be obtained from this type of
semen sample, procedures to extract sperm will not be used. The
sperm sample will be evaluated and processed to select only the
healthy, viable sperm for the fertilization
procedure.
When there is an absence of sperm in the
ejaculate, surgical extraction procedures are
performed.
One procedure called microsurgical
epididymal sperm aspiration, or MESA, is used when sperm are unable
to move through the genital tract due to uncorrectable blockage,
congenital absence of the vas deferens or seminal vesicles.
Aspiration is accomplished with MESA, usually performed as an
outpatient procedure, when sperm are extracted directly from the
epididymis. Epididymal sperm are typically not fully motile, which
means they cannot swim through the female tract to reach the egg for
fertilization. These sperm do contain the right genetic material,
nucleus and chromosomes, to produce normal babies. These sperm can
be used with IVF or ZIFT, assisted reproductive technology
procedures that place the sperm in direct contact with the
egg.
Sperm can also be aspirated from the testicles in
a surgical procedure called testicular sperm aspiration, or TESA.
These sperm are also typically not motile and mature, but do contain
the normal genetic material to produce normal
babies..
Step Three: Egg
Retrieval
This step is the same as in the other
ART procedures.
Step Four:
Micromanipulation and Fertilization with ICSI

Specially trained embryologists and
andrologists use micromani-
pulation techniques with the aid of
microscopic instruments to enhance the chances for fertilization. In
the laboratory, extra steps are taken with the eggs to remove the
cumulus cells that support the surrounding oocyte, or egg.
This
allows they embryologist and/or physician to visualize
the oocyte's maturity
and suitability to undergo the ICSI
procedure.
The semen sample is prepared, yielding as
many viable sperm as possible.
The goal is to locate as
many viable, healthy sperm as the number of selected eggs. While
transfer of multiple successfully fertilized eggs increases the
probability of success, ICSI has been proven successful with only
one viable sperm and one viable egg that are able to
fertilize.
Once an embryo is fertilized, it is
transferred back into the woman by injection into the uterus, as
with IVF.
Success
Rates
Definitive statistics have not yet
been published by the Registry of Assisted Reproductive Technology.
Preliminary success rates reported by various practices that offer
ICSI range from 15% to
35% deliveries per egg retrieval.
The American
Society of Reproductive Medicine Fact Sheet on ICSI
published
in December of 1996 states expected egg
fertilization rates of 50% and cleavage rates of 80% or more, but
only 15% to 20% of egg retrievals produce a delivery in well
selected couples. This Fact Sheet also states that perinatal
outcomes
studies in Europe suggest that although multiple
pregnancies are common in
ICSI, there is to date no
evidence of increased incidence of birth defects with this
procedure.
Your Guide:
Anna Peris, PharmD. -Stadtlanders' Fertility
Specialist
 ![]()
Sample Basal Body Temperature
Chart (BBT)
Charting your BBTs is really pretty
easy. Basically, what you are doing is taking your temperature first
thing each day and plotting the temperature on a chart. What you are
looking for is to see a shift of at least .4 degrees Fahrenheit
after ovulation making your chart biphasic (showing low temperatures
before ovulation in the follicular phase, and higher ones after
ovulation in the luteal phase).
- Take your temperature first
thing in the morning before you get out of bed or even speak --
leave your thermometer at your bedside within easy reach so you
dont have to move much to get it. If you use a glass thermometer,
make sure you shake it down before going to bed.
- Try to take the temperature
at as close to the same time each day as possible -- set an alarm
if you need to. Staying within a half hour either side of your
average time is a good idea because your temp can vary with the
time (i.e., if you usually take your temperature at 6 a.m., it is
OK to take your BBT between 5:30-6:30, but the closer to 6 the
better). The normal variation is by up to .2 degrees per hour --
lower if you take your temperature early, higher if you take it
late.
- It is best to take your BBT
after a minimum of 5 hours sleep, and at least 3 in a row is
preferable.
- You can take your
temperature orally, vaginally, or rectally -- just stay with the
same method for the entire cycle.
- You should try to place the
thermometer the same way each day (same location of your mouth,
same depth vaginally and rectally).
- Plot your temperature on
your chart each day, but refrain from reading too much into it
until the cycle is done.
- Some women, not all, have a
temperature drop when they ovulate. If you see this drop, it is a
good idea to have sex in case you are ovulating.
- What you are looking for is
a temperature shift of at least .4 degrees over a 48-hour period
to indicate ovulation. This shift should be above the highest
temperatures in the previous six days, allowing one temperature to
be thrown out as inaccurate (fluke, illness). Perhaps the best way
to explain this is to show an example.

In the image
above, the seven BBTs before ovulation are 97.2, 97.3, 97.8, 97.4,
97.2, 97.3, 97.0 then it jumps to 97.7 and then 98. Ovulation most
likely occurred on the day with the 97.0 and you can comfortably
draw a coverline at 97.6. You just ignore the 97.8 on day
10.
- After you see a temperature
shift for at least three days, or at the end of your cycle, you
can draw a coverline between your follicular phase and luteal
phase temperatures. With luck, it is easy to see a clear shift and
draw your line between the highest follicular phase BBT and the
lowest luteal phase BBT as in the sample above. The main reason
for drawing this line is just to clearly delineate that your chart
is biphasic.
- Look at the chart at the end
of the month to analyze what happened.
- Chart for a few months and
look for patterns.
- If your temperature stays up
for 18 days or more after ovulation, you should test for
pregnancy.
One thing to note is that women
with ovulatory cycles but with irregular cycle lengths, the greatest
variation from cycle to cycle should be in the follicular phase. The
luteal phase should be relatively constant (within 1-2 days). So if
one has a cycle that ranges from 28-34 days, and a luteal phase of
14 days, ovulation would occur somewhere between days 14-20 -- not
the middle of a cycle, not day 14 . . . This is the biggest mistake
women with long cycles make when trying to conceive.
Frequently Asked
Questions
Basal Body Temperature
Questions
Q: What will my BBTchart
tell me?
A: The goal is to find out if
you are ovulating and help you time intercourse. If you see a
definite biphasic chart, thats a good sign. You can also tell
whether your luteal phase is long enough if your temperatures are up
for at least 12 days after ovulation.
Q: How long should my
temperature stay up after ovulation?
Ideally, 14 days. Some doctors
say anything over 10 days is acceptable, but it really makes sense
to test for luteal phase defect if one typically shows 12 days or
less of high temperatures. You can test for luteal phase defect with
a serum progesterone level and/or an endometrial biopsy. Many
doctors will want to see two cycles of low progesterone or out of
phase biopsies before making a definite luteal phase defect
diagnosis.
Q: My temperature dropped
for a day in the luteal phase, does that mean this cycle is a
bust?
A: Not unless it stays down.
Some people have a short drop that may go well below the coverline
that is a secondary estrogen surge (which may be accompanied by
mucus).
Q: How long should I chart
before seeing a doctor if I suspect infertility?
A: Good question! If your
cycles are irregular, you shouldnt waste time on BBTs alone -- see
a doctor and find out what may be causing the irregularity. If you
do have normal-length cycles and decide to start charting, you only
need to wait about 3 months to establish a problem and seek help.
For example, if you have a 28-day cycle, but ovulate on day 18, and
that happens 2-3 months in a row, you should see your doctor.
Otherwise it depends on your age and urgency. Its not a bad idea
for everyone to get preconception advice and bloodwork -- test for
immunities to rubella, chicken box, fifth disease, also test for
anemia and thyroid function at a minimum.
Q: What are average
BBTs?
A: The average range of BBTs is
between 97.0-97.7 before ovulation and 97.7-99.0 after ovulation.
Ideally, a womans temperature will not bounce around more than .5
degrees in the follicular phase and will stay above the coverline
during the luteal phase.
Q: My BBTs are lower/higher
than average, what does this mean?
A: Either case warrants
checking your thyroid. Low BBTs are often a sign of hypothyroid
which can cause some fertility and pregnancy problems. Excessively
high temperatures may indicate hyperthyroid.
Q: I did and ovulation
predictor kit, how long after the positive should my BBT
rise?
A: You should ovulate 12-48
hours after the positive ovulation predictor test, and your BBTs
should go up within 48 hours of ovulating. It can take up to 4-5
days to see the rise, but ideally you see it within 3.
Q: My chart looks more like
the Rocky Mountains than anything else, what does that
mean?
A: Most likely a) you are not
taking your BBTs consistently or sleep erratically, b) you are
taking your BBTs orally and you sleep with your mouth open, or c)
you are not ovulating. If being more consistent, or switching to
taking your BBTs vaginally or rectally, doesnt help, you should go
to the doctor to have your hormone levels checked out and see what
may be causing your anovulation.
Q: How late in a cycle can
one ovulate?
A: It is possible to ovulate
very late in a cycle -- there is not any day limit -- so a long
cycle doesnt mean there is no hope. Long cycles do, however, reduce
opportunities to get pregnant and warrant looking into. It is also a
good idea to have at least one cycle every 3 months, brought on by
medication if needed, so that the uterine lining does not become too
thick.
Q: Can I tell I am pregnant
from a BBT chart?
A: You are most likely pregnant
if your BBTs stay up for 18 or more days after ovulation. It is also
common to see a triphasic chart, a second shift sometime during the
luteal phase, when pregnancy is achieved.
Q: Do I really need BBT
thermometer, or will a fever thermometer do?
A: A BBT thermometer is more
reliable and more accurate. In glass thermometers, fever ones are
only accurate to .2 degrees Fahrenheit. You really need it to be
accurate to .1 degrees. The main plus of the digital BBT over a
fever BBT thermometer is speed. The BBT digital is more accurate for
some people, and it only takes 30-60 seconds, which can matter if
you are waiting to go to the bathroom first thing in the morning.
The digital ones are harder to break and remember the temperature
for you if you dont want to chart it immediately.
 .gif)
|
